When planning began for a first-of-its-kind Urgent Mental Health Care Centre as an alternative to a failing emergency department experience, a new standard that centred people with lived experiences in system reform decisions was needed. People with lived experiences came together to co-create a philosophy of care for the centre that would uphold service integrity, hold implementation providers accountable, and communicate the care experience and service culture that people expect.
Innovation Summary
Innovation Overview
The what - People in the community want responses that are specifically prepared to understand and hold people experiencing Mental Health crisis/distress. Responses can be unavailable when needed, or public health responses such as Emergency departments are not always appropriate to respond to people’s needs. This can exacerbate the crisis and distress and break the trust between people and the systems that have been set up to support/protect them.
The innovation - The Office of the Chief Psychiatrist (OCP) in South Australia sought to influence doing things differently when moving into implementation planning for the new centre. TACSI and LELAN were commissioned to advise the OCP on how this could be done and suggested investing in creating a Philosophy of Care. This Philosophy was then co-created by a group of people who held specific lived experiences of crisis/distress emergency departments responses. The Philosophy of Care was a key reference document during the commissioning process in which people with lived experience participated in the evaluation panel that selected the service provider responsible for developing the Centre. It also provided key guidance for recruiting the Centre’s workforce, 50% of which comprises designated lived experience roles. The key innovation was the centring of their perspectives and leadership in how this centre would authentically come to fruition.
Objectives - This Philosophy of Care would name the principles that would guide the real-life implementation and specific service experience expectations and ultimately hold OCP and commissioned service delivery partners to account to deliver on what those with lived experience of crisis/distress want and need. This is a shift from an agency- to a person-centred approach that significantly impacts service modelling by meaningfully including the perspective of the community that will use the service.
Benefits - NEAMI is the organisation responsible for running the Centre, which is now operational 24/7, and has provided support to 5029 people who self-refer or are brought by police or ambulance as they were experiencing mental health distress in the community. "By the time I left, I felt renewed; I felt like I had aired out everything I needed to air out. It made me stronger, not just stronger, it made me who I am now" (source). Further, the service manager from NEAMI National recently told us that the Philosophy of Care “reminds us of the outcomes we need to be striving for, guides our values-based recruitment of centre staff, and ultimately keeps us accountable.”
Future - The philosophy of care has and will continue to guide the commissioning of similar services and/or lived experience-led expectations across local government and service providers. It is our aim to support the Philosophy of Care to be adapted to multiple systems reform settings.
The Philosophy of Care is a core underpinning document of other initiatives the OCP and other government and non-government agencies led, including the redesign of NGO-funded services, another Head to Health Centre in Adelaide’s North and a Safe Haven Cafe.
Innovation Description
What Makes Your Project Innovative?
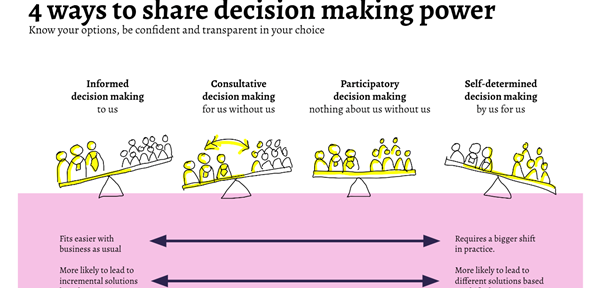
Traditionally mental health services are implemented through institutional leadership. This makes for little power, if any, to be shared with people with specific lived experiences and the community more broadly. The Philosophy of Care, however, was a shift up the participatory spectrum as the government was willing to share some power with people with lived experiences to set the course for the UMHCC. This meant that the government and a group of people with lived experiences worked as partners to share the decision-making of how the UMHCC would be the type of response people wanted and what this meant for people delivering the service. This is where the government moved to the ‘doing with’ community. This was an excellent example of a strategic partnership between government and civil society to promote citizenry participation and social inclusion of members of one of the most excluded groups of our community.
What is the current status of your innovation?
Currently, the Philosophy of Care is about to be adapted to a new crisis service that is due to be operational in 2023 in Northern Adelaide. The new crisis services in Adelaide are nested within bilateral agreements between Federal and State Governments; therefore, the philosophy of care as it stands and the adaptations to follow for the new crisis service has the potential to enable lived experience leadership across layers of the broader system, including the federal landscape.
Innovation Development
Collaborations & Partnerships
Why LELAN - We embody the knowing that lived experience matters and drive change through our voice, our influence and our leadership
Why TACSI - We partner with the whole system to enable a future where co-production is mainstream, new recovery and prevention solutions abound, and mental well-being is a whole society effort.
Why OCP - We are a statutory agency responsible for promoting continuous improvement in the organisation and delivery of mental health services in South Australia.
Users, Stakeholders & Beneficiaries
- People experiencing mental health distress and their families and friends
- Police and ambulance officers
- The lived experience workforce
- The mental health workforce
- Government and Civil society organisations
Innovation Reflections
Results, Outcomes & Impacts
The services collected systematic feedback from people receiving care using a patient-reported experience measure validated for the Australian population. This feedback is used for better governance and service improvement. The service plays a key role in hospital avoidance of Mental Health challenges by offering a suitable alternative to Emergency Departments. The following statements were provided by people who receive mental health care at the Centre: “The second night, I came back, and it was amazing. The peer workers, the light dimmers, the recliners, the snacks, and just feeling supported and SAFE. The communication on what is happening helped too.” “Peer Support Workers and the Nurse who looked after my arm without judgement. Knowing I could stay as long as needed and had safe transport home.”
Challenges and Failures
The codesigned project started when COVID hit South Australia, so the partner organisations were required to adapt to the new reality and develop a new efficient methodology to engage consumers and carers in a meaningful way. The Philosophy of Care brings a new way of providing mental health care underpinned by principles of autonomy and dignity of risk. This can conflict with the zero tolerance for risk perspective embedded in the sector. It required an open conversation to meet the essentials of the Philosophy of Care and the requirement of safety and quality inspectors.
Conditions for Success
- Government officers are available to work in partnership with civil organisations and participants in each coding process stage.
- IT capabilities to face the challenges related to the initial stages of COVID.
- A Consumer, Carer and Community Engagement policy with clear guidelines, including the reimbursement of people for their time, is essential in engaging the community.
- Government is willing to share decision-making power with people with lived experience to co-create the Philosophy of Care from the outset and announced changes stated in the philosophy of care at the launch of the new $14m Urgent Mental Health Care Centre (UMHCC) in Adelaide CBD on 3 March.
- The philosophy of Care was central to the commissioning of a delivery partner.
- The successful delivery partner had to prove how they implemented the Philosophy from the outset.
Replication
The philosophy of care became a reference for other strategic processes related to the mental health sector, including developing the workforce and new services beyond the crisis scope. During the SA Mental Health Act review, the philosophy has been a reference that was sent to the reviewers to understand the community's expectations regarding respecting their rights while receiving mental health care. The OCP has received feedback from other jurisdictions indicating an innovative approach to designing new services.
Lessons Learned
There is a growing movement that service design and implementation work better when exists an authentic partnership between multiple stakeholders who agree and commit to centring the involvement of lived experience. The philosophy of Care was an exemplary demonstration that partnership is possible.
Status:
- Identifying or Discovering Problems or Opportunities - learning where and how an innovative response is needed
- Generating Ideas or Designing Solutions - finding and filtering ideas to respond to the problem or opportunity
Date Published:
3 January 2023