IPJM offers a constructive tool for multi-disciplinary teams to work together in designing healthcare solutions, through mapping the physical and emotional journey of patients for both the current service and the proposed service reform. It supports groups in understanding and negotiating the conflicting requirements that can arise during transformational projects. This is achieved using journey mapping and user personas for graphically externalising key domain knowledge.
Innovation Summary
Innovation Overview
Health information technology (HIT) and associated data analytics offer significant opportunities for tackling some of the more complex challenges currently facing the healthcare sector. However, in order to deliver robust healthcare service improvements, it is essential that the design of HIT solutions considers in parallel the three core pillars of healthcare quality - clinical effectiveness, patient safety, and patient experience. This requires multidisciplinary teams to design and evaluate interventions that both adhere to medical protocols but also achieve the tripartite goals of effectiveness, safety and experience.
In this case study, a tool that has been developed during a healthcare project called LEANBH using a human-centred design research approach is described. The ‘Integrated Patient Journey Map’ (IPJM) assists multidisciplinary teams in designing effective healthcare solutions to address the three core pillars of healthcare quality. IPJM is unique in addressing the shortcomings of existing methodologies by supporting multidisciplinary practitioners working together using a visual tool to design healthcare solutions that consider not one but all three of Patient Persona, Patient Journey and Medical Pathway. This helps to ensure that the designed services meet the demands of existing constraints, performance improvement, and patient experience. Findings suggest that IPJM supports groups in understanding and negotiating the conflicting requirements that can arise during transformational projects. This is achieved using journey mapping and user personas for graphically externalising key domain knowledge. IPJM also promotes creative thinking around service reform goals and fosters dialogue among stakeholders, potentially leading to better solutions overall.
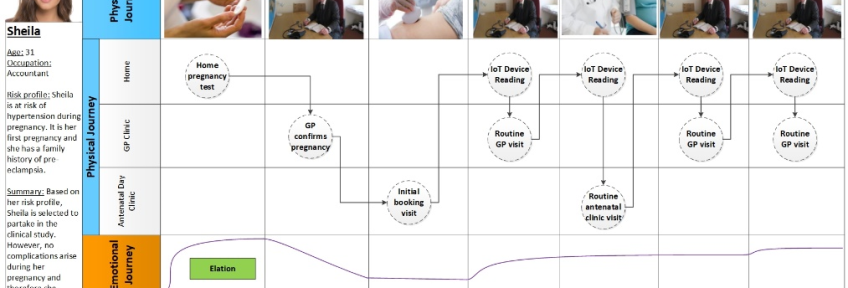
The LEANBH project team used IPJM during successive workshops to superimpose the journeys of fictional personas of different expectant mothers who would use the connected health service. Eight fictional personas were identified by the team to represent the different hypertensive disorders that can occur during pregnancy and the medical scenarios which can occur. This included ‘Sheila’, a 31-year old first-time expectant mother at risk of hypertension during pregnancy due to a family history of pre-eclampsia. Her journey through the standard antenatal pathway was now complemented with her use of the proposed connected health solution. Other personas included ‘Denise’, a 25-year old expectant mother who developed pre-eclampsia, and ‘Fiona’ a 29-year old expectant mother who developed gestational hypertension.
IPJM challenged the siloed thinking of both the clinical and IT subgroups. Individuals would often speak out on behalf of one of the personas and assert how certain decisions would affect the physical and emotional journey of this expectant mother. One powerful example of this emerged during discussions around the journey of ‘Brenda’, an expectant mother who (due to white-coat syndrome) is incorrectly diagnosed with gestational hypertension and admitted to the hospital. The group discussed the emotional impact this event would have on Brenda and challenged itself to come up with ways in which the connected health platform could be designed to avoid the unnecessary hospitalisation of Brenda.
As stated by the project manager, these activities represented a significant milestone where: “technical concerns and clinician concerns were starting to be addressed as a unit as opposed to being two separate entities… For the first time people realised that the journey wasn’t a clinical journey, it wasn’t a medical journey, but neither was it a technological journey. It was all combined together”.
Innovation Description
What Makes Your Project Innovative?
In comparison with other mapping tools, IPJM offers the possibility to focus on the comparison between the ‘AS IS’ and ‘TO BE’ versions of the pathway under study – this is a significant advantage in projects that pursue specific improvement targets. Findings indicate that IPJM offered a constructive tool for multi-disciplinary teams to work together in designing healthcare solutions, through mapping the physical and emotional journey of patients for both the current service and the proposed connected health service. This allowed team members to consider the goals, tasks, constraints, and actors involved in the delivery of this journey, and to capture requirements for the digital touchpoints of the connected health service. Above all else it helped to negotiate differences of opinion among stakeholders.
What is the current status of your innovation?
The IPJM has since been applied to numerous other contexts including palliative care, dentistry, and more recently antenatal visits in the era of COVID-19. A number of papers have been published on the IPJM and associated collaboration process. These papers were accepted in peer-reviewed outlets in both the healthcare and information systems domains. The following list provides a sample of papers for further reading:
• McCarthy, S., O'Raghallaigh, P., Woodworth, S., Lim, Y. Y., Kenny, L. C., & Adam, F. (2020). The 'Integrated Patient Journey Map': A Design Tool for Embedding the Pillars of Quality in Health Information Technology Solutions. Journal of Medical Internet Research.
• McCarthy, S., O'Raghallaigh, P., Woodworth, S., Lim, Y. Y., Kenny, L. C., & Adam, F. (2016). An integrated patient journey mapping tool for embedding quality in healthcare service reform. Journal of Decision Systems, 25(sup1), 354-368.
Innovation Development
Collaborations & Partnerships
The LEANBH project was a collaborative effort involving organisations from academia, the healthcare sector, and industry. Project partners included INFANT research centre (University College Cork), IBM, and Laya Healthcare. The creators of the IPJM are now looking for further collaborators to apply the IPJM to new clinical contexts and adapt the design tool to meet the demanding challenges currently facing the healthcare sector.
Users, Stakeholders & Beneficiaries
The IPJM provides a canvas for interdisciplinary groups to explore improved medical pathways, technical considerations of HIT platforms, and the needs and capabilities of different stakeholders e.g. expectant mothers, clinicians, developers, nurses, midwives, and other healthcare practitioners.
Innovation Reflections
Results, Outcomes & Impacts
The IPJM enabled the group to develop a common language around the antenatal pathway. It became a powerful means of building shared understanding. For example, the IS subgroup faced a steep learning curve to reach an understanding of the obstetrics domain and the various healthcare settings in which the connected health platform would be deployed. Similarly, clinicians had limited knowledge of the technology aspects of the connected health platform. The IPJM challenged siloed knowledge around the clinical and technology pathways and helped bridge disciplinary boundaries. The synergies arising from this confluence of disciplinary knowledge was essential for highlighting IT and clinical challenges, both previously known and unknown. As pointed out by the developer: “It was useful. It was only when I walked through the journey map explaining how the (smartphone) app would work that I realised that others had different interpretations”.
Challenges and Failures
It was difficult at times to secure participation from certain groupings in some meetings. For example, clinicians sometimes found it difficult to commit time to using IPJM as they felt they were too busy and that the journey maps were for the development team rather than for themselves. Resolving these misconceptions is essential to producing maps, which are accurate and robust in the face of real-life scenarios.
IPJM also does not make explicit reference to Key Performance Indicators (KPI) such as throughput and waiting times, or other metrics such as productivity and cost efficiency, although these may be essential elements of the performance and success of the services being designed. While incorporating this element in the tool would be useful, there is also a risk that increasing the level of detail may compromise the overall accessibility and reliability of the maps.
Conditions for Success
Shared understanding is crucial to the success of projects involving stakeholders from different organisational and disciplinary backgrounds. In the absence of shared understanding, the perspectives and intentions of team members can become increasingly fragmented as individuals may not even be aware of the intricacies of the issues around which they disagree. The IPJM provides team members with the opportunity to challenge assumptions embedded in ‘pre-baked’ project proposals and contribute diverse knowledge around the design of IT solutions. This helps ensure that design efforts promote both a shared understanding of users’ diverse needs and capabilities, and a commitment to the delivery of solutions that cater to these needs.
Replication
IPJM has been used by the Victoria Integrated Nephrology Working Group Project as a collaborative quality improvement approach to Patient Centered Care. The project engaged front-line staff and patients along with decision makers as partners in implementing practice changes to improve care. The IPJM contributed to the team being awarded a Celebration of Excellence (COE) Award in the Spring of 2018. The approach allowed them to engage “front-line staff and patients along with decision makers as partners. This structure has allowed the implementation of practice changes to improve care”. This promoted strong and respectful multi-disciplinary participation, relationship building, and provided a model for other interdisciplinary teams embarking on collaborative projects. IPJM is also recognised by the US FDA as an exemplar in how to take the patient experience into account when designing effective treatments. It is referenced in several of its guidance documents.
Lessons Learned
IPJM can be used as a cornerstone for modelling healthcare service reform where stakeholders collaborate to derive an understanding of and commitment to requirements. Benefits of IPJM identified in the LEANBH project include.
• Embeds pillars of quality - Considers clinical effectiveness, patient safety, and patient experience in tandem;
• Externalises knowledge - Allows stakeholders to externalise their domain knowledge and build a shared understanding;
• Stimulates creativity - Facilitates dialogue between different stakeholders around developing creative solutions;
• Accessible - Easy for multi-disciplinary stakeholders to understand, use and modify;
• Adaptable - Can be adapted to the requirements of different contexts and specialities;
• Emancipatory - Facilitates the alteration of medical pathways and the development of solutions for addressing their shortcomings;
• Educational - Acts as a platform for communicating proposed changes, and their impacts.
Anything Else?
Anyone interested in learning more about the IPJM or discussing future novel applications of the tool are welcome to get in touch. The programme offers consultation services on use of the IPJM, and is also actively looking for collaborators to develop the IPJM further in new contexts. If interested, please contact:
Dr. Stephen McCarthy, Lecturer, Cork University Business School, UCC
Email: [email protected]
Dr. Paidi O’Reilly, Adjunct Professor, Cork University Business School, UCC
Email: [email protected]
This work has emanated from research conducted with the financial support of Science Foundation Ireland (SFI) under Grant Number SFI/12/RC/2272.
Supporting Videos
Status:
- Identifying or Discovering Problems or Opportunities - learning where and how an innovative response is needed
- Generating Ideas or Designing Solutions - finding and filtering ideas to respond to the problem or opportunity
- Developing Proposals - turning ideas into business cases that can be assessed and acted on
- Implementation - making the innovation happen
Date Published:
18 March 2021