The city of Louisville has one of the highest asthma rates in the U.S. AIR Louisville was a community program that used smart connected inhalers to help improve the asthma problem in Louisville. AIR Louisville enrolled 1,147 citizens of Louisville to improve asthma for everyone. Citizens benefited by receiving personalized care. Louisville Metro benefited from crowdsourced, hyperlocal data of air quality challenges our residents face.
Innovation Summary
Innovation Overview
The AIR Louisville project equipped 1,147 residents with sensors for their asthma inhalers that tracks when, where and how often the inhaler is used. This information can help patients manage their symptoms. It can also help city leaders make smart decisions about how to keep our air clean enough to avoid asthma attacks in the first place.
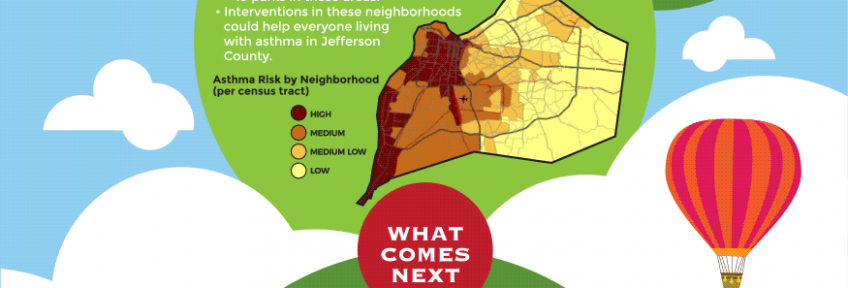
Using the data collected, AIR Louisville was able to create a map of asthma risk for each neighborhood in Jefferson County, based on the environmental conditions found in each region. AIR Louisville found that rescue medication use happened more often on days with higher temperatures and air pollutant levels, including: Nitrogen dioxide (NO2), ozone (O3) and sulfur dioxide (SO2).
The AIR Louisville team also has calculated the healthcare costs of living in polluted air. Based on the data collected from 1,147 participants, we can estimate the healthcare costs of a high ozone day. When ozone exceeds the EPA limit of 70 parts per billion, the community could expect to see more than 65,000 asthma rescue inhaler uses among all people with asthma in Jefferson County. That adds up to healthcare costs of up to $129,000 on just that day. In 2016, ozone exceeded the 70 ppb limit on 19 days, so those high ozone days could translate to more than $2.4 million in healthcare costs.
Innovation Description
What Makes Your Project Innovative?
In 2014, we attempted to measure air quality through low cost air quality sensors, but the data quality of the sensors was too poor. So we decided to use humans as proxy sensors and measure instead where, when, and how often rescue asthma and COPD inhalers were being used. We ended up crowdsourcing an enormous amount of data and combined it with environmental data to develop predictive models for asthma risk and now share those dynamic models with the public.
What is the current status of your innovation?
The project concluded in 2017: the final report out has been shared with the Robert Wood Johnson Foundation as the funding agency and numerous papers have been submitted to peer reviewed journals for publication. We hope that our learnings will be shared widely and that other institutions will adopt and adapt this work to address their own air quality challenges.
Innovation Development
Collaborations & Partnerships
The public served as citizen scientists, agreeing to share their medical information to better their community.
Government officials across multiple agencies worked together in novel, collaborative ways to act on the results of the project - traffic engineering addressed congestion through traffic light re-timings, sustainability worked to plant more trees, public health added their input on the impact for living/working/going to school near busy roadways.
Users, Stakeholders & Beneficiaries
- Enrolled citizens benefited from having a passive method to collect their rescue inhaler usage data and receiving personalized care to increase their asthma free days.
- Citizens throughout the city benefit from having cleaner air to breathe.
- Government officials, for the first time, have hyper local data about where air quality is a challenge and an use that data to create new policies.
The private partner, Propeller Health, had a large population to validate their product and ability to publish
Innovation Reflections
Results, Outcomes & Impacts
AIR Louisville helped participants improve their asthma and COPD. Over 12 months, we saw:
- An average of 82% reduction in asthma rescue inhaler use
- 29% of uncontrolled participants gained control of their asthma
- On average, AIR Louisville participants more than doubled their symptom-free days
- AIR Louisville participants slept better, with an average 19% increase in symptom-free nights
Many enrollees felt they received so much benefit from using the device that they requested permission to use it beyond the 12 month program.
Challenges and Failures
There was a subset of the enrollees who failed to use the device for the entire 12 month duration and experienced less of a positive impact.
It is also unclear whether or not enrollees need to continue to use the device or if they have developed long term behavior change for the better.
Conditions for Success
Part of the success of the Air Louisville project had to do with reciprocity among all stakeholders:
- Citizens had a free, super easy way to track actual rescue inhaler usage (traditionally, they are expected to keep a paper journal) and ability to track location, not just date/time
- Citizens received individual interventions (and remarkably, those interventions resulted in changes to health outcomes measurable by months, not decades)
- Propeller Health received a large scale platform to demonstrate the efficacy of their product and compensation to do so
- Louisville Metro received crowd-sourced, novel data to develop data-driven policies to improve air quality for all
- The Robert Wood Johnson Foundation had an innovative, breakthrough proposal aimed at improving the health for all
- Primary care physicians and respiratory specialists received accurate data to allow them to tailor the patient's treatments
Replication
We are in conversations with multiple cities and countries who face similar challenges with air quality and its impact of public health. They are interested in replicating the AIR Louisville project in their own communities.
Lessons Learned
Define the reciprocity of all stakeholders upfront.
Status:
- Diffusing Lessons - using what was learnt to inform other projects and understanding how the innovation can be applied in other ways
Date Published:
30 October 2014